You’ve probably heard the news: an FDA-approved treatment for sickle cell disease applying the gene-editing tool CRISPR is now available in the U.S. It’s a landmark moment in medical science on two fronts: the treatment, called Casgevey, is the first FDA-approved regimen to utilize CRISPR technology to treat any genetic disease. And it’s a huge leap forward in the treatment of sickle cell, a genetic disease affecting about 100,000 people in the U.S. — mostly African-Americans.
Today, we’ll delve into what this means for patients, learn more about the process they must undergo to receive a genetic sickle cell treatment, the little-known side effects of the process that affects their fertility, and how their fertility can be preserved.
Guests:
Manisha Bansal, MD, Hematology/Oncology, Nemours Children’s Health, Jacksonville
Vrunda Patel, MD, Pediatric & Adolescent Gynecology, Nemours Children’s Hospital, Delaware
Danielle Morley, BSN, RN, CPHON, Program Manager, Andrew McDonough B+ Fertility Preservation Program
Fredrianna Copeland Webster, advocate and sickle cell disease patient, Nemours Children’s Health, Jacksonville
Producer, Host: Carol Vassar
For more information on sickle cell disease, be sure to check out Episode 34 of the Well Beyond Medicine podcast.
Here’s Fredrianna Copeland Webster’s billboard, which may be seen across Jacksonville, Florida

EPISODE 45 TRANSCRIPT
Carol Vassar, podcast host/producer:
Welcome to Well Beyond Medicine, the Nemours Children’s Health Podcast. Each week, we’ll explore anything and everything related to the 80% of child health impacts that occur outside the doctor’s office. I’m your host, Carol Vassar. And now that you’re here, let’s go.
Fredrianna Copeland Webster, sickle cell disease patient and advocate:
I think any step forward in the treatment of sickle cell disease is amazing, and I’m always excited for it.
Carol Vassar, podcast host/producer:
That’s sickle cell patient and advocate Fredrianna Copeland Webster reacting to the announcement of a new and novel treatment for sickle cell disease. You’ve probably heard the news: an FDA-approved treatment for sickle cell disease applying the gene editing tool CRISPR, is now available in the US. It’s a landmark moment in medical science on two fronts. The treatment called Casgevy is the first FDA-approved regimen to utilize CRISPR technology to treat any genetic disease, and it’s a huge leap forward in the treatment of sickle cell, a genetic disease affecting about 100,000 people in the US, mostly African Americans. Today, we’ll delve into what this means for patients, learn more about the process they must undergo to receive a genetic sickle cell treatment, the little-known side effects of that process that affects their fertility, and how their fertility can be preserved.
Dr Manisha Bansal, Nemours Children’s Health:
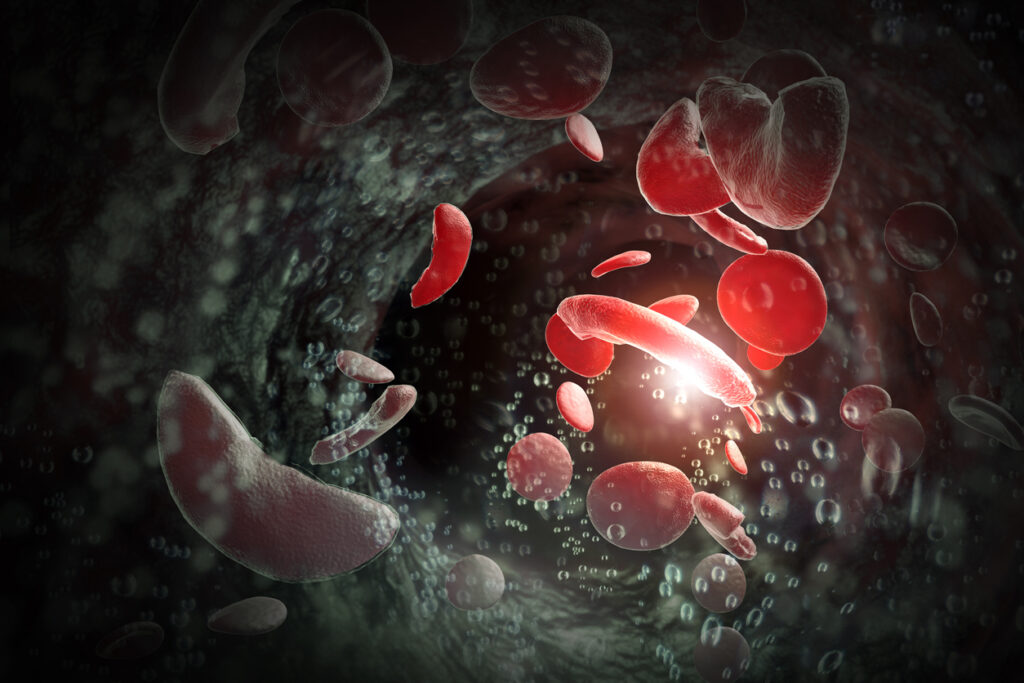
Sickle cell disease is a disorder of the red blood cell.
Carol Vassar, podcast host/producer:
Dr. Manisha Bansal is a board-certified pediatric hematologist-oncologist with Nemours Children’s Health.
Dr Manisha Bansal, Nemours Children’s Health:
It’s an abnormality, a genetic abnormality in a gene for the protein called hemoglobin. And hemoglobin is a protein that we all carry in our red blood cells and it’s the protein that carries oxygen from our lungs to the rest of our body. The tricky thing about hemoglobin is that it’s got a 3D structure to it, and there’s actually four pieces of it that bind together in order to carry the oxygen. And in sickle cell disease, what happens is that hemoglobin gene has a little tiny mutation in it, a little change in it that what it does is it affects the 3D structure of the hemoglobin. And that 3D structure abnormality is even more profound when there’s no oxygen attached to the hemoglobin. So essentially, after the oxygen is dropped off, the hemoglobin structure changes, and that structural change causes essentially a rod formation. So essentially, think about very firm rods in your red cells and think of red cells as kind of like a balloon. And so you have these rods that are changing the shape of the balloon, of the red cell.
Red cells are really needed to be very flexible and very malleable so that they can go through teeny tiny blood vessels. And so when there’s this structural change that leads to sledging and occlusion in certain blood vessels, and also these red cells don’t live as long, they tend to break very quickly. So, a typical red cell lives about three months, and a sickled red cell lives just a few weeks, two to three weeks.
Carol Vassar, podcast host/producer:
And the shape of it, if you were to put it under a microscope, it really does look like a sickle, doesn’t it?
Dr Manisha Bansal, Nemours Children’s Health:
It does. I mean, you can almost imagine very firm long rods in the middle of a balloon, and what that would do to a balloon, it would stretch it and kind of have pointy ends to it. And unfortunately, that structure is not very malleable, and so it will get stuck in various places and break more easily.
Carol Vassar, podcast host/producer:
And when it gets stuck, what happens?
Dr Manisha Bansal, Nemours Children’s Health:
So that’s the main problem. The two main problems with sickle cell disease is occlusion, so blockage, and then hemolysis, which is the destruction of the red cells. So the side effects or the complications of sickle cell that we typically think of are the ones that deal with occlusion, the blockage. And the most common one that people think about with sickle cell disease is pain episodes. If you can imagine these red cells getting clogged or blocked and the tiniest little blood vessels in a deoxygenated state. So after they’ve dropped off the oxygen, and the teeniest blood vessels you can imagine are commonly in the extremities and feeding bones and the back.
And so when this occlusion happens, you’re not actually able to deliver blood to those areas, and it can cause pain because you’re essentially not perfusing that area very well. That’s why when we talk about sickle cell disease, we say to avoid the cold weather because, in cold weather, your blood vessels will tighten up a bit to keep your body temperature where it needs to be. And so these same blood vessels then become even tinier, and it makes that blockage a little bit more possible.
The other complications of sickle cell disease that we commonly think of are acute chest syndrome, which is a pneumonia, but way more than a pneumonia. It’s a terrible cycle of less oxygen, destruction of red cells, inflammation, infection, and kids and adults can get very sick with that.
The last thing that we sometimes will think about with sickle cell disease is stroke, and that also has to do with vaso-occlusion because if you can’t deliver blood to the brain, then that area of the brain will be starving for oxygen, and that will cause damage to the brain in that area. So those are the biggest complications that we worry about in patients with sickle cell disease.
Carol Vassar, podcast host/producer:
So many chronic issues, including pain, the possibility of stroke, loss of lifetime, and lifetimes are shortened, are they not?
Dr Manisha Bansal, Nemours Children’s Health:
Correct. And that’s the hard part. It’s a difficult disease because it’s got chronic problems, but then also, out of the blue, out of nowhere, you’ll suddenly be dealing with a very serious complication that can affect your quality of life, either short-term, like a pain episode or long-term like a stroke. So it can be quite debilitating, and there’s really no way to know per patient what they’re going to face. I usually say you put ten patients with the same sickle cell disease the same genetics in a room, and every one of them will give you a different story of how sickle cell disease has affected them.
Because of that, either from the acute complications or the chronic complications that you see that develop over a lifetime of having sickle cell disease, an older patient with sickle cell disease will have a different story of how sickle cell disease has affected, will have significant complications, multiple physicians to visit, and quality of life being reduced. The lifespan of a sickle cell patient is definitely shortened. I will say, however, that with some of the newer medicines, such as hydroxyurea, that we have been doing a good job of prolonging the lifespan and the quality of life of patients with sickle cell disease.
Carol Vassar, podcast host/producer:
Which brings us to these new FDA-approved genetic treatments for sickle cell disease. And yes, there are actually two cell-based gene therapies now available for sickle cell patients. There is Casgevy, as noted earlier, using CRISPR technology to edit a patient’s DNA to switch on the creation of fetal hemoglobin, the production of which is significantly reduced starting after birth.
Dr Manisha Bansal, Nemours Children’s Health:
So the idea here is in the CRISPR technology is actually essentially gene editing. So the idea is to go in and to make small modifications to the genes that you already have and try to see if you can turn on or sometimes even turn off genes to manipulate essentially what the expression is of the different genes. What they’re actually doing is genetically modifying the expression of a different hemoglobin called fetal hemoglobin, and we typically call that hemoglobin F as in Frank. This is a hemoglobin that we all made before we were born. We made that instead of essentially the adult hemoglobin, which we typically call hemoglobin A, which is the non-sickle form. And then hemoglobin S is the sickle form.
So, the idea is to go back and increase the production of hemoglobin F, which we have the ability to make. It’s just been turned off when we were born. And so the idea is that this would be a way to turn the hemoglobin F back on, and that is a very favorable hemoglobin that functions just as well as hemoglobin A. So, by increasing the production of this in some cells, then the idea is we can shift the balance again to producing cells that are mostly hemoglobin F instead of hemoglobin S.
Carol Vassar, podcast host/producer:
There is also Lyfgenia, which uses a lentiviral vector to add a functional hemoglobin gene to a patient’s own blood stem cells.
Dr Manisha Bansal, Nemours Children’s Health:
With the lentiviral vector, what we’re doing is we’re actually inserting, we’re adding a hemoglobin that’s very similar to hemoglobin A that then that stem cell would express. So then that’s a way to actually turn on a better hemoglobin, but it’s not a hemoglobin that the patient already had in the genome.
Carol Vassar, podcast host/producer:
Whether it’s Casgevy or Lyfgenia, the patient’s treatment process requires the collection of their own blood stem cells for genetic modification and reimplantation, an autologous blood stem cell transplant. Autologous simply means the blood stem cells are collected from the individual sickle cell patient, no outside donor involved. That’s a plus because it eliminates the need to find a donor match, often a tall order. It also avoids the medical complications involved when receiving cells from someone other than the patient themselves. At the same time, the patient’s collected blood stem cells are undergoing genetic modification, their body is being prepared to host the reworked blood stem cells.
Dr Manisha Bansal, Nemours Children’s Health:
So, the idea is that you do have to give them chemotherapy. It’s called a conditioning regimen, which is high-dose chemotherapy to essentially make space for these new stem cells to be able to come in. The intention is not to wipe out every stem cell in the bone marrow but just enough so that these new stem cells can come in and make a home. It’s only one time that you have to get the chemo for the conditioning regimen. And after that, if this works, then not only are you spared any complications of sickle cell disease, but also not having to be on lifelong medications, which a lot of our sickle cell patients currently have to be on, such as hydroxyurea. So I think for quality of life, for longevity of life, and also for overall medical interventions in a lifetime, it could be very, very impactful.
Carol Vassar, podcast host/producer:
And yet, there are downsides to conditioning chemotherapy.
Dr Manisha Bansal, Nemours Children’s Health:
You are exposing these patients to drugs that can have side effects. There’s a lot of discussion about fertility issues later in life.
Carol Vassar, podcast host/producer:
Fertility? How does conditioning chemotherapy affect fertility? Dr. Vrunda Patel is a pediatric and adolescent gynecologist with the Andrew McDonough B-Positive Fertility Preservation Program at Nemours Children’s Health Delaware.
Dr. Vrunda Patel, Nemours Children’s Health:
The patients that are going to be undergoing these treatments have to undergo a conditioning treatment option prior to actually getting the genetic treatment, and that uses chemotherapeutic agents, which those medications can affect your ovarian reserve, which is the amount of eggs that you have in your ovaries. And so for sickle cell patients, they have to be able to receive that conditioning treatment first before they actually undergo the curative genetic treatment right now. So that can definitely impact your ovarian function and reserve for the future. And the same is true for males. It lowers the sperm count and thus can make patients unable to have their own biological children in the future.
Carol Vassar, podcast host/producer:
And the same is true for males. Conditioning chemotherapy lowers sperm count, making it unlikely for males undergoing the treatment to have biological children in the future. But can fertility be preserved? Dr. Patel says yes.
Dr. Vrunda Patel, Nemours Children’s Health:
So luckily, we have the options for fertility preservation here at Nemours, and a lot of that discussion we try to do as early on in treatment counseling as much as we can. And so for patients with sickle cell cancer, we try to do as early on in treatment counseling as much as we can. And so, for patients with sickle cell disease, we already know that their ovarian function can just be affected by their actual underlying sickle cell disease itself. And so, as teenagers, really, the gold standard of preserving fertility is freezing eggs. That technology has been well established; it’s been around for many, many decades, and that’s really the best offer that we have when you’re a teenager. And that relies upon having undergone puberty and having actual menstrual cycles.
But for kids who are younger, we cannot freeze eggs because it’s just not feasible for kids who haven’t gone through puberty. And so, for those kids, for girls, we talk about freezing actual ovarian tissue. So that would be a separate surgical procedure in which an entire ovary is surgically removed, and that tissue is then kept in storage in a freezer for later use. And right now that technology relies upon having a second surgery when they are older as adults and want to start a family. And that tissue is then re-implanted back into their bodies. And we have had documented pregnancies and live births following this technology in adult women. So, it’s an option that we do offer here at Nemours for girls who are pre-pubertal or have haven’t undergone puberty yet.
Carol Vassar, podcast host/producer:
And what about boys? How can their fertility be preserved? Nurse Danielle Morley is program manager for the Andrew McDonough B-Positive Fertility Preservation Program.
Danielle Morley, Nemours Children’s Health:
Yeah, so males who have gone through puberty, we offer sperm banking. We try to coordinate that with the times that they have not been previously exposed to some form of chemo. Sometimes, patients with sickle cell disease, before they go through a definitive therapy, get oral agents that can damage the sperm that’s in their body and thus make you not want to preserve that sperm. So sometimes, we’ll trial patients off of those drugs for enough time to be able to get good viable sperm from them prior to going through a more intensive therapy. And then for patients who have not gone through puberty, we do testicular tissue cryopreservation. It’s kind of similar to what Dr. Patel explained from the female standpoint, but we take out a portion of a testicle and cryopreserve it. The research is a little bit further behind for that, and they’re currently researching how to reimplant it, and there’s not currently any live births in human models, but hopefully, technology will continue to advance, and that will be a viable option for patients in the future.
One thing I just want to point out too, we are very fortunate here to be able to offer all these options. So we counsel any patient who’s going to be getting any type of chemotherapy, and we [inaudible 00:15:23] and tell them the level of intensity we think and likelihood of infertility based on the drugs they’re going to get. But this is not an option at every center. And so we are fortunate, and our patients are fortunate to be able to have these discussions and counseling and then opt to preserve if they would like to.
Carol Vassar, podcast host/producer:
Dr. Patel, many of these patients are underage. They’re not thinking about fertility. Maybe they’re even very young children. How do parents play into this decision-making process?
Dr. Vrunda Patel, Nemours Children’s Health:
I think the parents play a big role, but it’s really ultimately what the patient wants, especially when they’re at an age when they can voice their opinions. And for those patients, I think that joint decision-making happens within the family construct. For younger patients, the parents can help to make that decision, but also, as the child gets older, they can ultimately decide what to do with that tissue even when they’re older. So it doesn’t necessarily mean that they have to use that tissue, but they can decide where it goes and if it goes to research ultimately.
Carol Vassar, podcast host/producer:
So they have options.
Dr. Vrunda Patel, Nemours Children’s Health:
They do have options.
Carol Vassar, podcast host/producer:
What are some of the barriers with regard to fertility preservation?
Danielle Morley, Nemours Children’s Health:
Yeah, lots. I mean, there’s bigger ones like ethical considerations and cultural and religious, but on a more concrete thought of things, financial, insurance, time and how quickly we can do these things, and if they’re safe from a standpoint of what their body’s previously and recently been exposed to.
Dr. Vrunda Patel, Nemours Children’s Health:
And I think we’ve been really lucky that we’ve had a lot of philanthropic funding that’s been available for our patients and our families. So we have had several patients with sickle cell undergo some option for fertility preservation, whether that was freezing eggs or freezing ovarian tissue, and for the boys for freezing sperm. A lot of that depends on generous funds that we’ve received from surrounding families from organizations as well. We’ve also even had to write letters for insurance coverage. So we’ve written insurance coverage letters and asked for coverage for those procedures to be performed as well.
Carol Vassar, podcast host/producer:
So, some of this is covered by insurance?
Danielle Morley, Nemours Children’s Health:
Depends. Not as much as we would like to see. And it also depends on what type of insurance they have. There are some state mandates that were put into legislation in, I think it was 2018 in Delaware. So that has helped us a lot, but not all states have that. And even the Delaware bill doesn’t apply to all types of insurance.
Carol Vassar, podcast host/producer:
As for the newly approved genetic treatments for sickle cell disease, the estimated price tag is seven figures. Dr. Bansal.
Dr Manisha Bansal, Nemours Children’s Health:
It’s not cheap to do this. I’ve heard numbers around $1 million, $2 million for the entire endeavor, which is a lot. But then, if you weigh it compared to the cost of living with sickle cell disease, which is significant, I think it’s a justified cost.
Carol Vassar, podcast host/producer:
When asked about the possibility of undergoing one of the two available genetic treatments, patient and self-proclaimed sickle cell warrior Fredrianna Copeland Webster is both enthusiastic and realistic. Would this be something you would be interested in getting for yourself?
Fredrianna Copeland Webster, sickle cell disease patient and advocate:
Oh, yes, ma’am. Definitely. I think the barrier here is insurance coverage. I did my own research, and I found out that CRISPR is a multimillion-dollar treatment, and insurance coverage varies of course. I know a lot of people with sickle cell don’t have the best insurance coverage, so that’s a bit disheartening to me. But the point here is that some of us will be able to undergo this treatment, and I’m happy to hear that as opposed to this treatment not being available to anyone and the rest of us still being here living with sickle cell disease every day.
Carol Vassar, podcast host/producer:
Fredrianna Copeland Webster is a sickle cell patient and advocate. If you happen to be in the Jacksonville, Florida area, look for Fredrianna on highway billboards and at the airport as a stellar example of the scholars who attend Florida State College at Jacksonville, where her ultimate goal …
Carol Vassar, podcast host/producer:
…is to be a clinical researcher and find a universal cure for sickle cell and other cures for rare disorders. (Singing)
Carol Vassar, podcast host/producer:
Many thanks to our guests today, Dr. Manisha Bansal, Dr. Vrunda Patel, Danielle Morley, and Fredrianna Copeland-Webster, for sharing their expertise, insights, experience, and passion. And thanks to you for listening. If you’d like to see Fredrianna’s billboard or listen to the previous podcast episode featuring more of her personal sickle cell story, we’ll leave links in the show notes. CRISPR for treatment is now a reality. What do you think about this historic moment? Leave us a voicemail at nemourswellbeyond.org. That’s nemourswellbeyond.org, where you may also find our previous podcast episodes and get a chance to subscribe to the podcast and leave a review. Our production team this week includes Che Parker, Susan Masucci, Cheryl Munn, and Leah Goodwyne, with a special thanks to Dr. David Brousseau, pediatrician-in-chief for Nemours Children’s Health in the Delaware Valley, for sharing his medical fact-checking acumen. Join us next time as we talk about more ways that modern technology is enhancing healthcare, this time for the smallest of babies. I’m Carol Vassar. And until next time, remember, we can change children’s health for good well beyond medicine. (Singing).